Minimally Invasive Spine & Pain Interventions
Percutaneous Decompression Neuroplasty
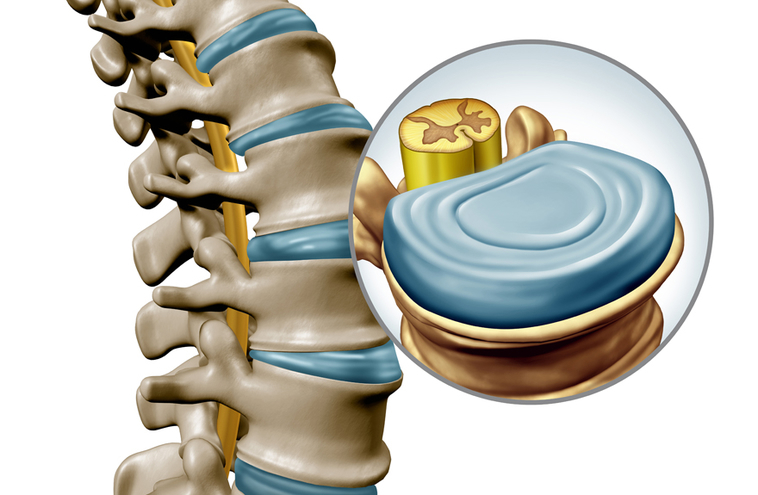
Except for direct compression of nerve structures owing to acute disc herniation or fractures of peripheral structures due to accidents, activation of chemical mediators is a key source of pain in most cases of spinal pain associated with degenerative changes.
What is Percutaneous Decompression Neuroplasty?
Percutaneous Epidural Neuroplasty (PEN), also known as percutaneous epidural neurolysis, percutaneous epidural adhesiolysis, or the Racz procedure, is a minimally invasive spine intervention that involves inserting a catheter directly into the herniated disc or scar tissue that is compromising the nerve root. PEN is used for epidural scar lysis, tailored medication distribution, ventral drug instillation, and neural decompression. A catheter is advanced to the location of adhesion, which is shown by an epidurogram, and adhesiolysis is done.
Percutaneous epidural neuroplasty (PEN) is a minimally invasive treatment.
Neuroplasty was first used to relieve back discomfort after spinal surgery. Its new indications are as follows:
- Spinal Stenosis
- Spinal compression fractures
- Inflamed or pinched nerves
- Degenerated, bulging, or herniated discs
- Facet joint syndrome is caused by degenerative changes in the spine
- Epidural inflammation or fibrosis
- Chronic pain following neck or back surgery
- Refractory back pain

